Why sleep matters
Sleep is a vital daily process just like eating and drinking. While sleep may seem like a simple activity, it has significant impacts on our health, happiness, and well-being. High quality sleep supports brain function, physical and mental health, growth, and recovery, whereas inadequate sleep or poor sleep quality can increase risk of diseases, exacerbate existing issues, and be detrimental to overall well-being. We want to help you understand what is high quality sleep, how to assess if you have a sleep problem, and provide resources and suggestions to help you improve your sleep and subsequently, your health and life!
Roughly 1/3rd of our lives are spent sleeping, so let’s learn what really goes on when we sleep and why it’s so important. Sleep can be defined as a state of lowered consciousness associated with distinct heart rates, breathing patterns, brain activity, and other physiological functions. While the body is not moving during sleep it is far from inactive. When you sleep, it allows your body to rejuvenate itself in many ways. For young children, sleeping is related to physical and mental development and maturation. For instance, in children ages 9-10 who got less than the recommended 9 hours of sleep per night, had more mental health and behavioral issues such as impulsivity, aggression, anxiety, and depression (https://www.nih.gov/news-events/nih-research-matters/children-s-sleep-linked-brain-development). Your prior night's sleep also affects your mood and mental health, and a good night’s rest can help you have the right mindset to approach your day. We also know that sleep is strongly related to the strength of our immune systems, so people who are sleeping better have a more robust immune system. Sleep is also related to our learning and memory consolidation. Moreover, lack of sleep is related to higher risks of high blood pressure, obesity, stroke, diabetes, and coronary heart disease.
It is worth noting that there are still many unknown or not fully understood aspects of sleep. For example, there is debate about why our bodies sleep; some hypothesize we sleep because it conserves energy–our bodies metabolism is reduced by 10% in our sleep, others believe that our body can repair and rejuvenate itself through sleeping, others think that sleeping during the night keeps animals safe, or that sleep allows our brain to reorganize, strengthen, and function. While we don’t yet have the question solved of why we sleep, there is no doubt that sleep is crucial to our health and well-being. Keep reading below to learn how you can assess and improve your sleep and subsequently, improve your health and longevity!
Keep reading below to learn how you can assess and improve your sleep and subsequently, improve your health and longevity!
Health Consequences of Chronic Sleep Loss
Most people think the only consequence of chronic sleep deprivation [<7hours a night] is daytime sleepiness. Nothing could be further from the truth. Chronic sleep deprivation results in impaired memory, impaired immune function, obesity in adults and children, diabetes and impaired glucose tolerance, cardiovascular disease and high blood pressure, anxiety, depression and increased accidents.
Sleep deprivation produces deficits in executive function [planning], increased difficulty in learning new information and a decline in working memory. Researchers believe that sleep is required for consolidation of memory. Without adequate sleep the brain has a harder time absorbing and recalling information.
The effects of sleep deprivation on the immune system range from increased risk of infection and decreased response to immunization to increased risk of cancer. A single night of short sleep can significantly decrease natural killer cells, the immune cells that fight cancer.

As average sleep amounts fell during the later half of the 20th century, obesity rates rose proportionately. When a person sleeps less than 7 hours a night there is a direct relationship between sleep loss and the degree of obesity. Sleep deprivation increases the hunger hormone, ghrelin and decreases the satiety hormone, leptin, therefore, the less you sleep, the more you are likely to eat.
Chronic sleep deprivation is now recognized as one of the major contributors to the rise of type 2 diabetes in the U.S. In the Sleep Heart Health Study, adults who slept 6 hours a night were 1.7 times more likely to have diabetes and those sleeping 5 hours a night or less were 2.5 times more likely to have diabetes. Some of this increase is due to weight gain but studies show that sleep deprivation led directly to impaired glucose tolerance.
How are Americans sleeping?
Even though the health risks of not getting enough sleep are clear, it turns out that Americans are not sleeping very well at all. CDC researchers reviewed data from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) and found that more than ⅓ of Americans are not getting the recommended 7 hours of sleep each night. Healthy sleep duration was lower among non-Hispanic blacks (54 percent) and multiracial non-Hispanics (54 percent) compared with non-Hispanic whites (67 percent), Hispanics (66 percent), and Asians (63 percent). People who reported they were unable to work or were unemployed had lower healthy sleep duration (51 percent and 60 percent, respectively) than did employed respondents (65 percent).

The prevalence of healthy sleep duration was highest among people with a college degree or higher (72 percent). The percentage reporting a healthy sleep duration was higher among people who were married (67 percent) compared with those who were never married (62 percent) or divorced, widowed, or separated (56 percent).
The National Sleep Foundation’s 2023 Sleep in America Poll found that the nation’s sleep health is strongly associated with the nation’s mental health. Half of all individuals who reported less than 7 hours sleep per night reported mild or greater levels of depressive symptoms.The study also showed that people with difficulties falling or staying asleep just 2 nights a week have higher levels of depressive symptoms than those without sleep difficulties.

The Sleep Cycle: What happens while we sleep?
When we are asleep, we are not merely unconscious, our brain goes through four distinct phases while we sleep and this cycle repeats about every 90 minutes throughout the night. There are two overarching categories of sleep stages: Rapid Eye Movement [REM] sleep and non-REM sleep. Non-REM sleep can be further divided into stages 1-4 by their distinctive brain wave patterns. Non-REM sleep comprises about 75% of the sleep cycle and is most prevalent in the first half of the night. In NREM sleep the body is in light or deep sleep and muscles relax and heart rate slows over about 90 minutes. During the deeper phases of NREM sleep the glymphatic system cleans the brain of waste products that build up during wakefulness. This process is thought to be important in preventing dementia. When the body enters REM sleep the mind is active and most dreaming occurs. The body is paralyzed during REM sleep so you don’t act out your dreams.. In one night, people usually will experience 5-6 cycles through all the sleep stages.. These cycles are affected by our daily habits and our environment. Indeed our day prepares us for our night’s sleep just as our sleep prepares us for the next day.
Circadian rhythm
Sleep is also intricately linked with daytime activities and our body’s “natural clock”, or circadian rhythm. Circadian rhythms are an intrinsic cycle that ebbs and flows through a 24 hour cycle of being awake or asleep. This rhythm influences melatonin production–which relates to sleepiness, core body temperature which fluctuates throughout the day, eating habits and more. The circadian rhythm is also influenced by external factors such as routine, light and temperature (see Shift Work and Jet Lag sections).
Circadian rhythms control our sleep-wake cycles and rhythms can differ between individuals, what we call different chronotypes. A chronotype refers to your body’s natural inclination to being awake and asleep at certain times, what you might call ‘morning or night people’. Chronotypes are really more of a scale than a dichotomy and are thought to be based on genetics, geography, age, and circadian rhythm. Knowing your chronotype and cultivating your life habits to align with your chronotype can help promote better mood, energy levels, sleep, and well-being. You can go to the Sleep Diagnostic Tools section and try out the Morningness-Eveningness Questionnaire here to find your chronotype (link).
Shift Work
People who work shifts at irregular times such as through the night or starting very early in the morning can cause a change in the body’s natural circadian rhythm because their activities and sleep patterns do not align with external cues such as natural light or standard eating times. People who do shift work have been found to get an average of 90 minutes less sleep per night. A misaligned circadian rhythm and work shift can result in mood swings, being more prone to mistakes, drowsiness, or even substance abuse if people turn to substances to try to influence their sleep-wake habits.
Tips for adjusting to shift work can include using blackout curtains, ear plugs, eye masks, and noise machines to support sleep at irregular times. It is also beneficial to establish a sleep hygiene routine (link to the section). Try to avoid reliance on caffeine to get through the shifts. Consider taking quick naps on breaks to maintain alertness (see nap section). Different shift schedules can affect individuals differently so it is important to adapt a schedule that works for you personally.
View the Shift work handout from the Sleep Health Foundation
- Melatonin has not been strongly shown to help shift workers adjust their sleep schedules. Read the scientific research
- Circadian rhythms, sleep deprivation, and human performance
Jet Lag
Jet lag is the misalignment between your “internal clock”--circadian rhythm–and external time cues. Jet lag often occurs with travel across different time zones, especially if they are very different times. Jet lag can result in sleepiness, impaired mental and physical function, issues with falling asleep, and more. The onset of jet lag is in the first few days after travel and symptoms may last for days up to weeks. Some methods to avoid the negative effects with jet lag include proactively altering your circadian rhythm/sleep schedule to align with the location you are traveling to, use light exposure to help adjust your circadian rhythm, avoid or minimize alcohol because it can disrupt sleep, strategically time caffeine consumption and exercise, limit daytime napping, bring items like a sleep mask and earplugs to help you sleep at night in the new location.
- Tips on How To Get Over Jet Lag Faster from the Sleep Foundation
- Mayo Clinic Handout on Jet Lag
- Tips for getting a good night's sleep

What is Enough Sleep?
How many hours per night is right?
People commonly ask, ‘how many hours of sleep is right for me’? It is important to know that at different stages of life, we need different amounts of sleep in order to be our best selves. The CDC provides specific recommendations by age group:
- 1-5 years old: 10-14 hours (including naps)
- 6-12 years old: 9-12 hours
- 13-18 yo: 8-10 hours
- 18-60 y: 7+ hours
- 61-64: 7-9 hour
Differences with aging
We require different amounts of sleep at different stages of life. Generally, people’s sleep quantity decreases over time and plateaus around age 60, and the same pattern applies to naps. Sleep efficiency, which can be defined as a ratio of time asleep and time spent in bed, decreases as we age. Older people also tend to wake up more throughout the night. Studies have found that nap frequency increases in older adults. As people age, they also report lower sleep quality. Sleep is also influenced by lifestyle, socialization, medical comorbidities, and environment–all of which differ greatly across the lifespan.
“Sleep in Normal Aging” research publication
“Aging and Sleep” by Sleep foundation
Sleep quality
Sleep quality encompasses how well you are sleeping and while there is some overlap. It is possible to sleep a full 8 hours, but still have a poor sleep quality.. Sleep quality also includes self-satisfaction with sleep. While quality is harder to measure, ease of falling asleep, timing of sleep during the day, and alertness during the day can all relate to sleep quality. Sleep quantity can be measured using actinography, polysomnography, or sleep detection apps, and assessment also usually includes subjective assessment. Sleep quality has been linked to well-being and daytime sleepiness (https://pubmed.ncbi.nlm.nih.gov/9226606/) and improved mental health (https://www.sciencedirect.com/science/article/pii/S1087079221001416).
How to Feel Energized & Sleep Better With One Morning Activity | Dr. Andrew Huberman
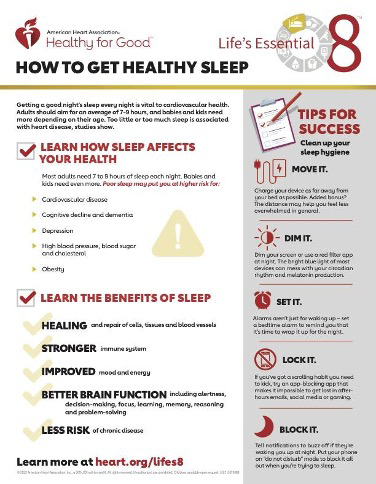
Sleep hygiene focuses on habits, environments, and routines during the day and at bedtime and focuses on adjusting these practices to help encourage sleep. This includes things such as going to bed and waking up at consistent times, not using electronic devices before going to bed, keeping your sleep environment at a cool temperature and dark, avoiding caffeine in the afternoon and more. Sleep hygiene is sometimes considered to be a first-line treatment for someone struggling with insomnia and good sleep hygiene is the key to a good night’s sleep.
Some recommendations for your sleep hygiene include:
- Establish a regular bedtime routine, bedtime, and wake up time
- Create a relaxing bedtime routine which might include a warm bath or shower, reading a book, listening to calming music
- Dim the lights in your sleeping environment as you prepare for bed
- Avoid being in bed besides when you are actually trying to go to sleep
- Avoid caffeine and limit alcohol in the hours before you go to sleep
- Exercise in the afternoon, at least 3-4 hours before bedtime
- Avoid large meals before bed
- Remove electronic devices from your sleeping environment and try to avoid using these devices in the hour prior to bedtime
Sleep Hygiene Flyer from the Centre for Clinical Interventions
How To Practice Good Sleep Hygiene from the Clay Behavioral Health Center
How to assess my sleep?
Do I have a sleep problem?
Sleep disorders in the United States are largely undiagnosed and undertreated. Signs of a sleep issue include daytime grogginess, fatigue, difficulty concentrating, weakened immune system, loud snoring, or breathing difficulties (skip to sleep apnea section here), or tingling feeling in legs. It is important to prevent, recognize, and treat sleep disorders because they are related to higher rates of diabetes, cardiovascular issues, obesity, as well as contributing to issues such as car accidents and depression.
Sleep assessment tools
You may know you are having trouble with your sleep but often we are so accustomed to being chronically underslept that we don’t even notice. Several tools are available to help you assess your sleep.
Epworth Sleepiness Scale:
This scale asks respondents to rate how sleepy they feel doing various daily activities. Respondents add up their responses and use this score to help determine if there is potential concern regarding their sleepiness.
Try out the Epworth Sleepiness Scale
More information about the Epworth Sleepiness Scale and how to score it.
The Pittsburgh Sleep Quality Index (PSQI)
The Pittsburgh Sleep Quality Index (PSQI) is a self-rated questionnaire which assesses sleep quality and disturbances over a 1-month time interval. It can be used as a simple screening measure to identify “good” and “poor” sleepers. A PSQI global score of >5 indicates significant sleep difficulties. The instrument and scoring instructions are at the end of the paper.
Insomnia Severity Index (ISI)
This validated screening tool takes about 5 minutes to complete and includes seven questions about the self-perceived severity of sleep difficulties, how it interferes with daily life, distress about the sleep problem where respondents respond using a 5-point scale. Scores are tallied to determine the severity of your insomnia. Try out the ISI yourself here. This is also accessible through the FREE CBTi Coach app.
Morningness-eveningness questionnaire (MEQ)
This app asks users 19 questions about their habits and what times they do certain activities and then tells you your “circadian rhythm type” [chronotype] and informs you about the associated melatonin onset, estimated natural bedtime, therapy that can help aid in better sleep based on your type. The online questionnaire is easy to use and they automatically calculate your score and give you the results immediately!
OSA STOP BANG
This tool is useful for assessing if you might be experiencing Obstructive Sleep Apnea using quick questions about if you snore, your age, BMI, gender and a few other items. The website calculates your score and determines if you are at low, intermediate, or high risk of OSA. If your STOP BANG score is in the high risk category, you should talk with your doctor and consider getting testing to determine if you have sleep apnea. You can consult the George Washington Sleep Medicine page here.
Try out the scale OSA STOP BANG Scale
If you are at high risk of having a sleep problem, it is advisable to see a sleep specialist for a home polysomnogram. A healthcare provider might also recommend keeping a sleep journal and could use data from wearable technology (link) to understand your sleep disorder more. You can consult the George Washington Sleep Medicine page here.
What if I’m not happy with my sleep?
If you are not happy with your sleep,explore potential reasons for your sleep issues, your sleepiness and insomnia severity, or your chronotype and discuss these findings with a medical professional.
- Begin by trying to optimize your sleep hygiene (link to section).
- The next step would be to try CBT-i therapy (link), which is accepted as first line treatment for insomnia.
- If you think you are experiencing another sleep disorder besides insomnia, talk to your doctor.
Sleep disorders
It is estimated that 50 to 70 million people in the United States have ongoing sleep disorders. A sleep disorder, also known as a sleep-wake disorder, can be defined as involving “problems with the quality, timing, and amount of sleep, which result in daytime distress and impairment in functioning” (APA). Interestingly, the prevalence of sleeping disorders began to spike with the invention of the lightbulb! As people started to utilize unnatural light patterns, this altered sleeping habits and the hours people sleep at night. In our current day, there are other external factors such as screens, social media, sleeping pills, and more which can significantly impact our sleep. Below we will describe key features of common sleep disorders. You can also read more in depth about sleep disorders from the Sleep Foundation here.
Some general red flags which might be indicative of a sleep disorder include:
- Falling asleep without meaning to
- Feeling sleepy or groggy even if you sleep 8+ hours
- Regular difficulty waking up or falling asleep
- Having issues concentrating
- Snoring or irregular noises during sleep
- Mood swings during the day
Insomnia
Insomnia is a continual difficulty falling asleep and/or staying asleep. People with insomnia often struggle with daytime sleepiness and can develop stress over their inability to sleep, which can compound the issue. It is estimated that around 10-15% of the US population has chronic insomnia, with a slightly higher predilection in women than men. The underlying cause of insomnia has not been identified and in order to diagnose insomnia, other sleep disorders must be ruled out first. Acute insomnia lasts for less than 3 months and can be related to stressful life events often, whereas chronic insomnia persists for longer than 3 months.

Cognitive behavioral therapy for insomnia (CBT-i)
CBT-i is currently accepted as the first line treatment for insomnia (https://www.acpjournals.org/doi/10.7326/m15-2175). CBT-i is a psychosocial health intervention that focuses on thoughts, beliefs, and stress about sleep and aims to replace those with sleep-promoting thoughts and attitudes. Cognitive Restructuring is the aspect of CBT-i which aims to shift the focus away from negative thoughts and emotions associated with sleep because of past experiences. Stimulus Control uses classical conditioning techniques to associate the bedroom and bed itself with sleep; so, people should avoid relaxing, reading a book etc in their bed. Finally, Sleep Restriction limits the time spent in bed so that by staying awake and active longer, they will actually be tired when getting into bed and fall asleep quicker.
“Cognitive Behavioral Therapy for Insomnia” Stanford Medicine
“How Does CBT-i work?” by Stellar Sleep
Sleep Apnea
Sleep apnea is a condition in which people experience breathing disturbances when sleeping, commonly resulting in snoring, gasping, or choking for air and waking up from sleep. The most common type of sleep apnea is obstructive sleep apnea (OSA) in which the upper airway muscles inappropriately relax and block breathing. OSA is highly underdiagnosed, with roughly 20-30 millions of people in the US having sleep apnea, but almost 8-90% of these cases are undiagnosed. People with sleep apnea might not realize their difficulties breathing or might not remember waking up throughout the night, however, they feel very tired during the day. The risk of sleep apnea increases with age and can be worsened with alcohol and caffeine, as well as obesity.
OSA is treatable in nearly all cases so diagnosis is important. Treatment options include CPAP, dental appliances and surgical options. The most common treatment is a Continuous positive airway pressure (CPAP). This device covers your nose and mouth as you sleep and maintains enough air pressure so that the airway remains open. Here is a useful 11-page handout titled “A Good Fit: Making CPAP Work for you” which walks readers through how to use a CPAP and how to comfortably incorporate this useful technology into their lives.
Narcolepsy
Narcolepsy involves excessive daytime sleepiness, despite sleeping enough at night, along with “sleep attacks” of a strong urge to sleep and often, actually falling asleep temporarily without warning. This can occur during normal daily activities such as walking around, working, or driving. These attacks can also be accompanied by muscle weakness in which a person may collapse or slump over. As a result, narcolepsy can be potentially dangerous for the individual and others around them. It is a relatively uncommon disorder that is estimated to affect about 1 in 2,000 people. Onset of narcolepsy is usually around 15 to 35 years of age. It can be challenging to diagnose narcolepsy and it can go undiagnosed for years. There is no cure for narcolepsy. Behavioral symptom treatment approaches include practicing sleep hygiene, taking short planned naps, avoiding sedatives, exercising cautions with driving a car or operating machinery. Pharmacological treatments include stimulants to aid in staying awake throughout the day.
Restless Leg Syndrome (RLS)
RLS is the sensation of tingling or crawling which causes a strong urge to move one’s legs. It can also involve aches and pains and makes it difficult to fall or stay asleep. RLS affects 5-10% of adults and 2-4% of children. RLS can be alleviated by walking around or massaging one’s legs so being active can be protective against RLS. RLS can occur alongside other conditions such as pregnancy, parkinson’s disease, iron deficiency anemia and neuropathy. Some scientists believe RLS is linked to dopamine which helps control muscle activity. Dopamine receptor agonist drugs have been shown to decrease RLS symptoms. Alcohol, caffeine, and nicotine can all make RLS worse. Other prevention and treatments for RLS can include compression therapy, exercise, massages, and hot baths.
NIH Health Information: Restless Leg Syndrome
Mayo Clinic Handout: Restless leg syndrome
Other Sleep Disorders
You can read about other sleep disorders such as sleepwalking, night terrors, excessive sleepiness and more here on the Sleep Foundation website.
Frequently Asked Questions (FAQs)
- Naps
-
Opinions on the role of napping and sleep are mixed. When you sleep, you go through a normal sleep cycle (light, deep, REM sleep) and depending on the duration of the nap, you can wake up at different stages of the sleep cycle. This can result in feelings of grogginess.
Pros and Cons of Napping
PROs
- Short naps (5-15 minutes) have been linked to feeling more alert, reduced sleepiness, increased cognitive function (Link to the study)
- Naps (30-90 minutes) have been linked to better word recall, which is related to memory consolidation
- Naps can help compensate for lack of sleep whether that be because of schedule, jet lag, etc.but cannot completely make up for lost sleep.
- Naps can improve mood
CONs
- Feeling groggy or disoriented after the nap
- Disruptions of nighttime sleep, harder to fall asleep at night
Take Home Points
- Naps cannot serve as a substitute for a proper night’s sleep
- Naps are not a solution for chronic insomnia or other sleep disorders such as obstructive sleep apnea
- It is a bad sign if you are taking naps because you cannot get through your day otherwise
- Naps are OK if they are short, in early afternoon and don’t interfere with nighttime sleep.

Resources:
- Alcohol and Caffeine
-
Alcohol
There is a common misconception that a “nightcap” alcohol drink before bed can help people fall asleep and while alcohol initially acts as a depressant which may aid in falling asleep, as your body metabolizes the alcohol this effect dissipates disturbing the sleep architecture (the structure of a normal night's sleep) and REM especially. Drinking alcohol can cause people to wake up more and feel less rested in the morning. Alcohol is also a diuretic and can result in a greater need to go to the bathroom, and contribute to waking up. Moreover, alcohol can increase snoring which is particularly harmful to people with OSA. So, if you choose to consume alcohol, have your last drink at least 3-4 hours before bedtime.
- Research publication that compiles lots of recent research on alcohol and sleep
- Sleep Foundation article about Alcohol and Sleep
- EverSleep article about how Caffeine Affects Sleep
Caffeine
Caffeine is a natural stimulant which acts to block adenosine receptors, which normally would promote sleep, which explains why caffeine results in alertness. Coffee, for example, has a half-life of about 5-6 hours and it takes your body around 10-12 hours to fully process the caffeine in a cup of coffee. So, you can see how an afternoon cup of coffee could majorly affect your body’s ability to sleep at night. Similarly to alcohol, caffeine can disrupt your natural sleep architecture and it acts as a diuretic. People who have insomnia, didn’t rest well, or work shifts might turn to caffeine to help with daytime drowsiness, which further exacerbates the sleeping issue when they try to sleep the next night. It is advisable to limit daily caffeine intake, only consume caffeine in the morning, and avoid reliance on caffeine to combat tiredness and underlying sleep or medical issues.
Screen Time
Electronic devices are ubiquitous in today’s society and unfortunately, devices can be very harmful to people’s sleep. Devices with screens emit light that stimulates alertness, therefore disrupting the circadian rhythm. Studies have found that light from devices within two hours of going to bed can disrupt sleep. It is important to try to reduce screen time before going to sleep in order to achieve longer duration of sleep and increased ease of falling asleep.
- Sleeping Pills
-
The use of sleeping medications is relatively common and it is important to understand how these pills work, associated risks, proper dosages, and how to avoid unhealthy reliance on pills in your sleep routine. In the National Health Interview Study conducted in 2020, 8.4% of participants used a sleeping pill in the last 30 days and 6.3% of adults took a sleeping pill every day in the last 30 days.
Melatonin: Melatonin is a natural hormone that our body produces as part of our natural circadian rhythm associated with sleeping and can be taken as a supplemental pill. The recommended dosage is 0.5-2 mg; however people frequently take far higher doses than is necessary or optimal. While some people believe increasing the dose of melatonin increases its effects, this is not true.
Melatonin can cause drowsiness so beware to not operate a vehicle within 5 hours of taking melatonin.
Trazodone: An antidepressant which blocks histamine and increases serotonin and results in drowsiness in around 30 minutes, therefore it is used off-label for insomnia. A regular dosage is about 25-100 mg. Trazodone is helpful for racing thoughts and does not disturb sleep stages and it is not addicting.
Barbiturates and benzodiazepines: This sedative drug category acts to calm the brain but has the most potential for harm and interferes with sleep stages, suppressing deep sleep which results in feeling less rested and refreshed. Barbiturates are an older type of drug which can be used to anesthetize patients or to treat epilepsy and are not recommended for long term usage for insomnia (should not be used for more than 2 weeks). They also have lots of drug interactions and can cause withdrawal. Benzodiazepines can be prescribed by a doctor for anxiety or sometimes for insomnia and are not recommended for long term use (more than 4 weeks). However, there are significant risks associated with benzodiazepines. Notably, they have been found to be related to increased all-cause mortality.
Resources to learn more and improve your sleep habits
Jump to: Apps | Wearables | Podcasts/Movies/Videos | Scholarly Resources | Books | Useful Websites
Apps
|
All iPhones have access to a free Health app which can set sleep times and goals and then suggest times to go to sleep and wake up to meet goals. The app charts your ‘Time in Bed’ based on your iPhone usage at night. |

|
|
This app is designed with children (0-10 years old) in mind and has a database of children’s bedtime stories, sounds, and music designed to aid in children’s bedtime routines to help them fall asleep. It is also possible to record a bedtime story for them in your own voice! Feedback has shown that the app can assist in shortening the time it takes children to fall asleep, as well as fewer parents perceived sleep problems. |

|
|
Provides self-hypnosis sessions to help users with stress relief, insomnia, and pain perception. Guided sessions designed by Dr. Seigal, M.D., a psychiatrist who has worked at Harvard, Yale, and Stanford. Describes hypnosis as a naturally occurring state of highly focused attention which allows an increased ability to control one’s mind and body, which can be harnessed to help with things like sleep. Their website also includes links to lots of scientific research articles and sources about hypnosis and sleep: https://www.reveri.com/sleep. |

|
|
Based on cognitive behavioral therapy approaches designed for insomnia patients to use along with seeing a health provider. Techniques which have been shown to be effective to help users fall asleep and stay asleep. Includes a “Sleep 101” section, a section which focuses on sleep habits such as designing a sleep environment or strategies to help fall asleep when experiencing insomnia and another section which provides strategies and resources for helping relax the body and mind like breathing tools or imagery guides such as through a forest or beach, as well as a diary to track sleep habits. Other sections include preventing insomnia and sleeping with a partner. App users choose a section they would like to explore and can view tips, inspiring messages, relevant advice and some sections are interactive where users indicate problem areas and get customized advice. There are also several assessment tools with customized insight to your insomnia and how to improve it. |

|
|
Headspace App Headspace provides a wide range of meditations, calming stories, and sounds as well as techniques to focus on stres relief, intention, awareness, and more. They provide research and articles for users to learn about calmness, managing stress, and sleep. They also feature some movement classes such as yoga. Headspace is free to download and has some freely accessible features and costs $12.99 per month or $69.99 annually. |
|
Wearables
|
Oura ring |
|
|
The Apple Watch allows users to set bedtime sleep schedules and how many hours users want to sleep per night and estimates time spent in each sleep stage–REM, Core, and Deep–as well as when it suspects you may have awoken. The watch requires 4 hours of sleep recorded per night to provide insight data and shows trends for the previous night and average trends over the past 14 days. The watch measures respiratory rate but notes “Respiratory Rate measurements are not intended for medical use.” A common limitation of the watch is that users take off their watches to charge at night. |

|
|
The Whoop strap is a faceless wearable tracker that uses photodiode sensors to monitor your everyday activities, including sleep. The strap provides information about hours of sleep needed, time in bed, hours asleep, sleep stages, wake events and provides recommendations based on recent sleep. Data is provided nightly as well as trends over the last 30 days. Research findings have shown that the strap performed reasonably well compared to polysomnography (A validation study of the WHOOP strap against polysomnography to assess sleep https://pubmed.ncbi.nlm.nih.gov/32713257/) and shown promising results indicating that the strap can help users achieve higher sleep quality (https://pubmed.ncbi.nlm.nih.gov/32043961/). |
|
|
Fitbit creates various models of health trackers such as wearable straps with clocks and smartwatches which connect to smartphones. The tracker uses heart rate and movement to tell you your sleep duration, sleep quality, and ‘restoration’--how relaxed you were in your sleep based on your HR. The device also gives you a score (0-100) and makes recommendations. Some devices can also detect snoring and other noises to see how noise affects your sleep. The Fitbit has shown to be comparable to polysomnography and useful for assessing changes in sleep quality over time or in response to interventions (https://pubmed.ncbi.nlm.nih.gov/31718308/). |
|
| The research article ‘A Validation of Six Wearable Devices for Estimating Sleep, Heart Rate and Heart Rate Variability in Healthy Adults’ (https://pubmed.ncbi.nlm.nih.gov/36016077/) assesses the Apple Watch S6, Garmin Forerunner 245 Music, Polar Vantage V, Oura Ring Generation 2, WHOOP 3.0 and Somfit. The overnight laboratory study demonstrated that all 6 devices were valid for timing and duration of sleep, but all needed improvement in distinguishing the sleep stages. | |
| Wearable activity trackers-advanced technology or advanced marketing? https://pubmed.ncbi.nlm.nih.gov/35445837/ |
Podcasts/Movies/Videos
|
The Power of Sleep: A lifestyle Medicine Approach by Dr. Param Dedhia (1 hour 23 min) (freely accessible) |

|
| The Matt Walker Podcast (45+ episodes, each around 10-15 minutes, general and specific topics) (freely accessible) Ex. #01 What is Sleep?, #07: Naps, #35 Sleep and Memory Pt. 1, #46 Sleep and Teens The Matt Walker podcast has 45+ episodes that range from about 10-45 minutes with a general discussion about sleep or a specific aspect of sleep. Feel free to peruse the episodes and listen to leading sleep expert Matt Walker discuss topics of interest to you. |

|
| Importance of Sleep with Daniel Dickson (Podcast episode, 26 minutes, PhD in Clinical Psychology) This 26 minute podcast with Danial Dickson, a PhD in Clinical Psychology, discusses sleep, how it changes across the lifespan, and tips to improve sleep quantity and quality using a CBT-i informed approach. |

|
| Science of Sleep Dr. Michelle Oliathe TEDxMandurah (13 minutes) This 13 minute TED Talk discusses interesting research findings about sleep deprivation, as well as relations to mental and physical health, and explains some of the mechanisms of sleep, and how you can “wake yourself to death but sleep yourself well”. |

|
|
Audio to Help with Falling Asleep: These audios include guided meditations and calming sounds which are designed to help with falling asleep. |
Scholarly Resources
| Sleep and Health—A Lifestyle Medicine Approach Param Dedhia, MD; Robert Maurer, PhD Introductory overview about the critical link between sleep and health as well as treatment approaches. |
|
| Sleep Difficulties in Adults: United States, 2020 Dzifa Adjaye-Gbewonyo, Ph.D., Amanda E. Ng, M.P.H., and Lindsey I. Black, M.P.H. Provides information about prevalence of sleep disorders and how this varies in different populations. |
|
| Sleep timing, sleep consistency, and health in adults: a systematic review Jean-Philippe Chaput et al. A systematic review assessing the relationship between sleep and health outcomes. |
|
| Healthy Sleep from Division of Sleep Medicine at Harvard Medical School |

|
| Improving and Maintaining Healthy Sleep Habits from University of Wisconsin Madison School of Medicine and Public Health 11-page overview document with links to all cited research papers. |

|
Books
| Why we sleep: unlocking the power of sleep and dreams Matthew Walker Describes developments in sleep research up til recent years including the importance of sleep for longevity and health, external influences on sleep such as environment, caffeine, and jet lag. It also explains different sleep stages, how sleep changes across the lifespan, dreaming, and how we can maximize our sleep. |
| Say Goodnight to Insomnia: The 6-week program Gregg D. Jacobs, PhD A program developed and validated at Harvard based on Cognitive Behavioral Therapy interventions (CBT-i) which has been shown to be more effective than drug-based approaches to fixing insomnia. Focuses on addressing lifestyle to help promote better sleep, eliminating dependency on sleeping pills, and positive thinking. |
| The Sleep Solution: Why your sleep is broken and how to fix it W. Chris Winter, MD Demonstrates the essential link between sleep and healthiness, how to establish a helpful sleep routine, describes the psychology and neuroscience of insomnia and how to overcome obstacles to good sleep. |
